Although Audiology is Not Rocket Science, We Do Take Care of Rocket Scientists
The Most Trusted Hearing Experts in North Alabama
Your journey to better hearing is like the Space Race in the 1960’s. It took more than a rocket to put a man on the moon. Apollo 11 required the knowledge and commitment of NASA scientists and engineers.
At Alabama Hearing Associates, we know that the right technology combined with the right audiologist makes all the difference!
Hearing loss creates a barrier to good communication, causing the brain to work overtime trying to understand speech. Our goal is to reconnect you to the people you need to hear, so that you can continue to meet your personal goals and live your best life.
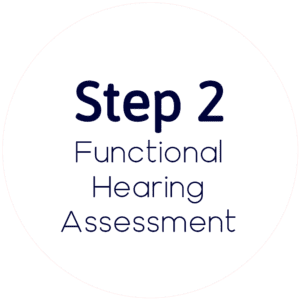
Prescription hearing aid technology and audiological best practices established by industry leaders are at the core of our treatment recommendations.
This methodical, evidence-based approach to hearing healthcare reunites you with friends, family, and colleagues so that you feel confident tackling each and every day.
With offices in Madison and Huntsville, you have access to Alabama’s most trusted Doctors of Audiology.
If you are ready to take the first step, call us today at (256) 319-4327 (Madison) or (256) 489-0903 (Huntsville).
Alabama’s Most Trusted Hearing Care Experts

Do You Struggle to Understand Speech in Noise?
Hearing loss can affect anyone, at any point in life, and can be triggered by a number of biological and environmental factors. A common warning sign for hearing loss is the inability to understand conversations in noisy social situations and restaurants.
If you struggle to understand speech in noise, we recommend scheduling a Functional Hearing Assessment. Unlike a basic hearing test, our Functional Hearing Assessment is a comprehensive communication evaluation, from ear to brain.
The Latest Prescription Hearing Technology
Our community understands better than most what can be achieved when you combine technology with human intelligence and persistence. It is much the same with hearing technology.
The latest prescription hearing aid technology is incredibly powerful, offering stellar sound quality and performance. Wireless connections allow phone calls, music and television to stream directly to your hearing aids for exceptional clarity.
But prescription hearing aids do not fit and program themselves! For best outcomes, you also need the human touch and expertise provided by our Doctors of Audiology.

Listening With Your Brain
At Alabama Hearing Associates, we don't just treat your ears, we treat the whole person. While your ears collect sound, your brain is what interprets it into meaningful speech. In other words, you hear with your ears, but you listen with your brain.
Studies show a strong link between age-related hearing loss and accelerated cognitive decline. Long-term hearing deprivation can affect cognitive performance, especially in complex listening environments.
It is often the small things that hold us back from making a decision. That’s why we are on hand to help.
Simply complete the Callback form to request a friendly, no-obligation conversation with one of our helpful team members.
Don’t want to wait? Call us at: (256) 319-4327
What Our Patients Say
About 7 years ago, I began to realize I was saying ‘What?’ a lot when others spoke to me. I couldn’t catch every word on the TV, and I avoided calling my family who all live in other states.
– Carolyn Seeley
I realized that I had a hearing loss when I had to ask people to repeat themselves almost all the time. My husband also asked me one night if I could hear the bird outside our bedroom window.
– Diana Dowdy
My husband kept telling me I needed to do something. I kept asking him to repeat himself. But when I finally admitted I needed help was when I noticed I wasn’t hearing my customers.
– Janice Hudgens
I became concerned about my hearing when I started not hearing the doorbell ring when I was in the bedroom. My sons noticed and said, ‘Mom, you don’t hear anything!
– Jeannie Anderson
I started having hearing challenges in 2003. I was still working at that time and I was concerned how colleagues might respond to my situation. Dr. Susan was the first audiologist I saw.
– John (Jack) L. Smith
“I realized I had a hearing problem when I was in a meeting with two co-workers. I could not understand what they were saying. At home, I had trouble hearing my husband and the TV.
– Julie Brown
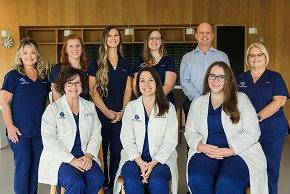
Meet The Team

Dr. Susan Sheehy
Doctor of Audiology
Dr. Jan Liles
Doctor of Audiology

Dr. Sarah Kate Fisher
Doctor of Audiology

Dr. Brianna Thomas
Doctor of Audiology

Pam
Insurance Specialist

Stephanie
Patient Care Coordinator

DeAnn
Patient Care Coordinator

Laura
Patient Care Coordinator

Chris
Account and HR Manager

Sonya
PATIENT CARE COORDINATOR

Gabby
AUDIOLOGY ASSISTANT
Patient Resources
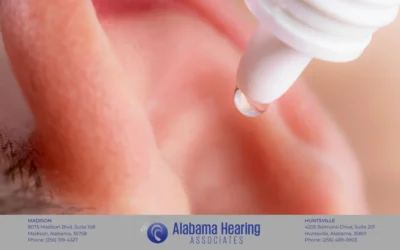
Understanding Ear Wax Removal: A Comprehensive Guide
Ear wax, medically known as cerumen, is a natural substance produced by the glands in the ear...
Best Way to Clean Ears
As practicing audiologists, we are frequently asked about the best methods for cleaning ears....
How To Use Earwax Removal Drops
While often overlooked, earwax plays an important role in protecting our ears from dirt, debris,...
YOUR JOURNEY TO
BETTER HEARING